Liver Transplant and Surgery
Who needs a Liver Transplant
According to international guidelines, any patient suffering from liver cirrhosis who is assessed to have a life expectancy of less than a year should be considered for a transplant. Severity of liver disease is graded from A to C. Usually all Grade C and most grade B patients are candidates for transplant. Any patient with any of the liver failure symptoms listed below should seek specialist opinion so that liver experts can assess whether a transplant or drug treatment is more suitable for them. In any case, the better the condition of the patient at the time of transplant, the better are the results of surgery. In patients who are critically ill in ICU, malnourished, have active infection, or other organ damage such as kidney impairment at the time of the operation, the results of transplantation are dismal. Therefore, timely transplant is of essence in obtaining good results. A timely transplant done on a patient who is in a reasonable condition, with a good donor liver has around 80% chance of success.
In most instances, the above causes initially result in Hepatitis which can usually be treated. However, if the offending factor is not removed or treated on time, cirrhosis develops and then it is usually too late to change the course of the disease.
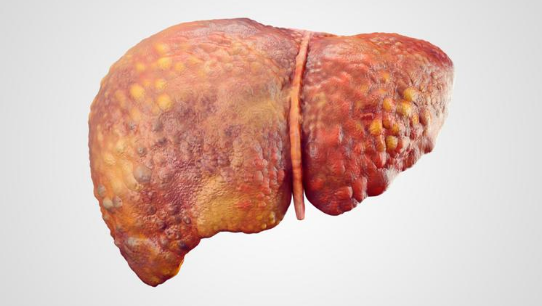
Symptoms of liver failure due to cirrhosis
- Black stool
- Blood vomiting
- Water in the abdomen (ascites)
- Drowsiness and mental confusion
- Excessive bleeding from minor wounds
- Jaundice
- Kidney dysfunction
- Excessive tiredness
- Low hemoglobin and other blood counts
Pre-transplant evaluation (Liver Transplant Assessment)
The liver specialist usually suggests this evaluation once he has diagnosed end-stage liver disease. Recipient evaluation is done in three phases and normally takes 5-7 days in hospital.
To establish definite diagnosis, determine the severity of liver disease and the urgency of the transplant.
To determine the fitness of the patient for a transplant. The other systems such as heart, lungs, kidneys, blood counts are tested and the presence of any infection is ruled out. The liver specialist then decides how successful the surgery is likely to be depending on the status of the patient and the cause and severity of liver disease.
The final phase entails the psychological and mental preparation of the patient. The patient and the family are counselled about the procedure, hospital stay, the likely course after surgery, follow up and aftercare.
After evaluation, the patient is either placed on the waiting list for cadaveric donation, or, if there is a willing and blood group matched family donor available, he/she is evaluated for donation and a transplant is scheduled.
While on the cadaver waiting list, the patient follows up with the Transplant Team until a suitable liver becomes available. If the patient's condition shows signs of deteriorating, we normally suggest the family to consider living liver donation.
Liver Transplant Operation
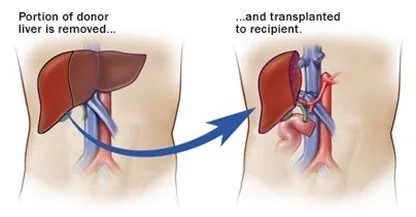
Live Donor Liver Transplant
Living donor liver transplantation is the process in which a healthy person donates a portion of his liver for the patient whose liver is completely damaged. This type of transplantation uses the feature of liver regeneration. The remaining liver gets regenerated in the donor while the transplanted liver portion grows into a complete liver in the recipient. The liver is divided into various segments and grafting of a segment is done depending upon the requirement of the patient. Such type of liver transplant reduces waiting time, flexibility in the schedule of surgery and increase the survival rate. Research indicates that people who have a liver from a living donor have a high survival rate as compared to people who get the liver from a deceased donor. Success rate of 97 %.
Recipients who are eligible for getting a liver transplant can opt for a living donor transplant. It is important to note that a suitable matching (ABO matching) is preferred for successful transplant outcomes.
Cadaveric donor (deceased donor) liver transplant
Deceased donor or Cadaver liver transplant: It is the most common liver transplant process. In this type of transplantation, the liver to be transplanted comes from a deceased donor. The donor may either have cardiac death or brain death. Strict guidelines are followed to certify a patient as brain dead. Braindead patients do not have any brain function but the other organs including liver are in good condition. Sometimes the patient has low brain function and is not fulfilling the criteria of brain death, however, with the consent of the relatives, the life support system of such patients can be removed. In such a case, the death is not considered as brain death rather a cardiac death. Livers obtained from the cardiac death patients are at increased risk of organ dysfunction, biliary complications, and thrombosis of the hepatic artery.
Cadaver liver transplantation is in practice from many years. In this case the liver of deceased person who is declared brain dead, after the complete evaluation of the donor his liver is safe for transplantation can be transplanted to a patient with liver problem. In hospitals, patients with liver problem register themselves for Cadaver transplantation and these patients are kept in waiting list until a cadaver liver donor is available.
The waiting time can be very variable from 1 to 12 months depending on your blood group and your waiting list number. While waiting, if you are not available at your usual numbers, you must inform the Transplant Team of your whereabouts at all times so that they can contact you as soon as an organ becomes available.
It is good idea to have a suitcase already packed with essential toiletry and underwear at home so that no time is wasted before you go to the hospital.
Split liver transplantation
Split liver transplantation involves splitting the liver obtained from a deceased donor to two patients requiring liver transplantation. Split liver transplantation increases the number of cadaveric grafts.
Preparing for Surgery
When you arrive at the hospital, you will undergo a series of tests. These are a routine part of the preparation for surgery and are designed to discover any infections which may not be immediately obvious. You will have a general physical examination and be asked to give samples of urine and blood. A chest X-ray, and electrocardiogram of your heart will also be made. Finally you will be asked to wash yourself thoroughly with antiseptic soap and the nurse will shave the surgical area.
The transplant surgeon and anaesthetist will meet with you to explain the operation procedure and the risks that may be involved. You will be asked to sign a form consenting to the operation.
The Operation
The transplant involves a major operation to remove the diseased liver and replace it with a normal donor liver placed in its usual position in the right upper abdomen. While this may sound relatively easy, the surgery is very demanding and can take between six and eighteen hours to complete. At least three surgeons, two anaesthetists, and half a dozen nurses are needed during the operation. The diseased liver must be disconnected from four major blood vessels and the tube that carries bile from the liver to the intestines, known as the bile duct, has to be disconnected from the bowel. The new liver is then put in place, and the major blood vessels and bile duct reattached to complete the operation.
Post Operative Care
After the operation you will be taken to the intensive care unit and connected to a respirator (breathing machine). If all goes well, the respirator can gradually be phased out over 24-48 hours, although it is not unusual to require the respirator for longer periods of time.
After three to ten days in intensive care, you will probably spend another two to four weeks convalescing in the transplant unit before being allowed to go home. It is important that you try to get up and about as soon possible so that blood circulatory problems can be avoided.
Since the donor liver is foreign to the body, the body mounts an immune response to reject it. This is prevented by certain medicines referred to as immunosuppressive drugs.
After another one month at home, you will start feeling normal again and gradually be able to get back to normal activities. Once the donor liver takes in the body (if the person remains well for about 3 months after operation), the person has an excellent chance of leading a normal life and with longevity comparable to any other person of their age and fitness.
Check-up Visits
During the first 3 months after discharge from the hospital, it is important that you return to the Transplant Unit once or twice a week for follow-up visits. The purpose of follow-up visit is to monitor your progress and detect any potential complications. On each visit, your liver function will be carefully assessed and you will undergo an examination so that any infections can be identified. Once you are stable, the frequency of visits will decline.
Living with a Liver Transplant
Going Home
Going home after a transplant although a happy occasion, may be accompanied by a significant level of anxiety for the first few weeks. Despite the potential problems, the majority of transplant patients return to a normal lifestyle and activity within three months. They work, have a family, raise children, play a useful role in the community and enjoy recreation.
Best Diet and Nutrition for Healthy Liver after Liver Transplant
You have been ill for a long time prior to your transplant and have probably lost a lot of weight. Therefore eating properly is an important part of your recovery process, and a healthy and balanced diet will help get you back on your feet again.
Your diet should include:
- Fruits
- Vegetables
- Whole-grain cereals and breads
- Low -fat milk and dairy products or other sources of calcium
- Lean meats, fish, poultry, or other sources of protein
Further recommendations:
- Weigh yourself every day
- Avoid sugary snacks such as cakes and biscuits between meals. If you feel hungry, eat some fruit or vegetables (low in calories).
- Try to drink about 2 litres of fluid every day. This is good for your kidney and help remove waste products from your body. Bottled mineral water, herbal teas, pasteurised low-fat milk, and fruit juices are good.
- Always wash and peel fresh fruit
- Vegetables that grown in soil, eg potatoes, should always be peeled and cooked in boiling water. Cooking vegetables in a pressure cooker is a good way of saving the vitamin content. Do not eat raw vegetables, eg lettuce.
- Do not eat cheese made from unpasteurised milk and avoid cheeses with mould.
- Only buy small amounts of dairy products at one time so that you can eat them while they are still fresh.
- Salt (Sodium).
While on steroids, try to restrict your salt intake by:
- Using salt sparingly when cooking
- Trying not to add salt to cooked food or salad
- Avoiding salty foods, eg potato crisps, pickles and tinned food
Exercise
It is important to have daily exercise routine to build up your muscles weakened by a long of illness. You should slowly increase your levels of exercise. Cycling swimming, and walking are very useful for increasing your stamina and overall muscle tone, and all going well, you can also resume other sports three months after the operation.
Before starting on any exercise programme, remember to check with your transplant team.
Driving
It is not advisable to drive a car during the first four weeks following transplantation.
Alcohol
Alcoholic beverages are not recommended. Alcohol is broken down by the liver and can cause live damage.
Smoking
Stop smoking! Smoking is harmful to everyone's health.
Sexual Activity
You may resume sexual activity as soon as you feel well enough. The majority of men regain their potency and most women find that their menstrual cycle returns to normal a few months after the operation.
Fertility
Many men have successfully fathered children after transplantation, and a large number of women have given birth to healthy children. Women should discuss their wish to start a family with their doctor or a member of the transplant team.
Normally, you should wait at least a year before becoming pregnant. Furthermore you should have good kidney function, be free of any illnesses which could endanger your or your baby's health, and be receiving low dose immunosuppressive therapy.
Vacation
There is no reason why you should not enjoy traveling provided you use common sense. You should always take enough medication with you for the whole trip. Always leave an address where you can be contacted.
Household Pets
It is not normally recommended to have household pets because of the increased risk of infection.
